Written by jason reynolds Low back pain is the number 1 cause of doctor visits in the U.S. aside from the common cold. Low back pain is an epidemic and it will affect 85% of us at some stage of our life and to varying degrees. Low back pain however, is a garbage can term; it is both ambiguous and useless if we do not define the specific pathophysiology that would manifest the label of “back pain.” Now one thing that needs clarification is that the chronicity of low back pain seen in the average American is often different than the acutely episodic low back pain an athlete may encounter. Some of the same anatomical, physiological and biomechanical principals are true of all lumbopelvic injuries or “back pain,” still it remains that the etiology and prognosis will vary from your athlete to your, relatively speaking, unfit individual. A perfect working example of this is the recently inured yet fast healing patient and colleague, Chad Smith the Juggernaut. This 3-part article serves as a journey and case study into the cause, management and prognosis of “back pain,” the often elusive, multifaceted, number 1 cause of disability in the US. Hopefully we can unravel some truths about the causation, progression and appropriate therapies in dealing with such a menace to our society.
This is the long-time-coming, conclusive 3 of 3 article addressing rehabilitation of the lumbar spine. This series has stretched over the same amount of time that would be comparable to a full, 100% recovery from a traumatic, non-surgical disc injury. To bring yourself up to speed or if you have yet to read my first two articles, I suggest you check them out here to prime your brain for the information in this article. Lumbar Spine Rehab-Part 1 (Assessment) and Lumbar Spine Rehab-Part 2 (Passive Care). In part one I dissect through the epidemiology of “back pain,” and explain the importance of movement preparation and functional integrity of the lumbar spine. In part two we journey through the passive therapy world and look at the tools used to assist the bodies fight to normalcy. In this last article, we will look at the keystone piece of rehabilitating the lumbar spine and any neuromusculoskeletal injury for that matter, active care.
The biggest disservice that any healthcare practitioner could provide is an allopathic approach to disease and dysfunction. In its most denotative sense, allopathy relates to the treatment of symptoms rather then the cause of the symptoms; the connotation of allopathy is usually associated with mainstream medicine (drugs and surgery). As more and more people are looking to other non-allopathic means of healing or treating their disease and dysfunction, the practice of allopathy is leaking into the ranks of conservative, holistic and alternative care practitioners. The best example of this is a Chiropractor only manipulating the spine, or a Physical Therapist using only active care exercises. I know this is very black and white but I am not suggesting that every practitioner provide every treatment modality possible, but a tunnel vision approach is a formidable path and fact remains that “allopathic” conservative care is just as chronic a problem as allopathic medicine. Active care is typically the most important and the most lacking component of a therapy plan for neuromusculoskeletal injuries and dysfunctions. We explored the idea of General Physical Preparation (GPP) in my Part one article, and how a body needs to be prepared for whatever demand you will be imposing on it. In the unfortunate event that the integrity of your body’s tissues is compromised by its inability to withstand imposed demand, there is a need to both evaluate the GPP state of the body and devise rehab that returns the body back to a pre-injury state. Here is where a holistic approach to rehabilitation is a determining point in how effectively the body bounces back to a state of normalcy.
Active care is defined simply as exercise. From a clinical perspective it is in broad sense rehabilitation. Active care has its place in all types of healthcare environments. It has its definitive place in more systemically based dysfunctions such as cerebral pathologies or cardiopulmonary pathologies but most of the healthcare worlds active care is performed in the orthopedic world. So if you have tendonitis, or a ligament sprain, arthritis, or back pain chances are some type of active care is being performed. The undermining of active care in a treatment plan has varied degrees, since we will be reviewing the active care plan that was utilized for Juggernaut Chad Smith’s lumbar disc herniation lets look at some of the plans that could have been presented to Chad on his road to getting back to pre-injury status. Let me preface this critique by stating that all of these approaches are correct assuming they are part of a plan and progression not the stand-alone active care approach. In order of least effective to most: First of all a plan without active care and only passive care like the plan discussed in Lumbar Spine Rehab-Part 2, would be insufficient on its own. The next tier could have been a stretching regimen, the old advice of just stretch and rest. I’ll even give the benefit of the doubt that this theoretical stretching advice includes adjacent areas, so for the example of lumbar spine rehab, we will include the hip complex, beneficial but not close to optimal. The next tier would be a specific stretch such as Williams’s flexion protocol or McKenzie’s extension protocol. These are two very effective active care approaches that are specific to different types of disc pathology, but with these alone, a palliative affect is the best result and functional deficits will remain. Strengthening would be the next approach and yes its true the more adaptive to external stresses the more resilient a tissue becomes to pathologic change, the garbage can notion of “strengthen your core” is a great adage but lets be honest what is your core and how do you effectively strengthen it? Then comes the last tier of what I consider an “allopathic” approach to rehabilitation and that is functional training. Although in its denotative meaning yes absolutely this is what we need to accomplish but from the overwhelming connotative sense in the healthcare industry functional training means gizmos and gadgets, and skill challenging exercises rather then, well, function for that individual. As I stated, all these “tiers” of rehab are potential components of a well-rounded holistic approach to rehab. If you have a comprehensive plan the only thing between your patient/client and optimal health is their compliance.
Constructing a rehab plan for any individual starts with the diagnosis or if you are not a doctor, the assessment, as described in Lumbar Spine Rehab-Part 1. Now we do not need to go into depth on diagnosis and assessment but it is fair to reiterate that knowing exactly what the injury, dysfunction and pain generating factors are, half of the battle can be won. I want to begin by trying to change the paradigm on what rehabilitation really is. This is something I compulsively try to convey to patients in my clinic and clients that do performance training with me. It is also what I based all of my teaching on when I taught active care and rehabilitation at the Southern California University of Health Sciences. Hopefully I am preaching to the choir with this statement but rehabilitation is an event that is training the body’s neurology PERIOD. If at any stage you start talking about strength, or explosiveness, or flexibility you have just crossed out of the rehabilitative world and into the performance world. PERIOD. If we take a look back at the idea of preparedness or GPP, these building blocks are a series of neurologic events coordinated through efferent execution (you telling your body to produce a movement or action) and afferent feedback (the body telling you all systems go) to produce a movement, or activation or relaxation etc. A perfect example of this neurologic phenomenon is the ability to diaphragmatically breathe and maintain an active, relatively neutral lumbopelvic spine (and a major part of Chad’s rehab). As you read this now I want you to try this (this is a diagnostic assessment clinically used). Place one hand on your chest and one on your stomach. Tighten your core (however you see fit to do that) now take a deep breathe. Chances are your superior hand on your chest travelled vertically more so then your inferior hand on your stomach travelled horizontally. This is pathologic breathing and you too would benefit from breathing rehab. Ventilation should be completed through the diaphragm being contracted and flattened through the ventilation phase all while you are maintaining a protected, relative neutral lumbar spine. Below I will take you through an abbreviated approach to the beginning acute phase weeks of conservatively rehabilitate a lumbar disc herniation. I will attempt to describe the exercise and its conceptual and theoretical reasoning to how it fit into the plan for Chad, and his functional needs.
BREATHING:
As I used in the above example breathing was a huge part of Chad’s rehabilitation, especially in his more acute phase in the first couple weeks. With the help of other specialists in the Juggernaut community, Chad connected with Molly Galbraith Check her out online and Ryan Brown check out this breathing video. Together we helped change one of Chad’s fundamental components when loading the spine. Please check out these links above for more detailed info on Chad’s breathing component.
LUMBOPELVIC CONTROL:
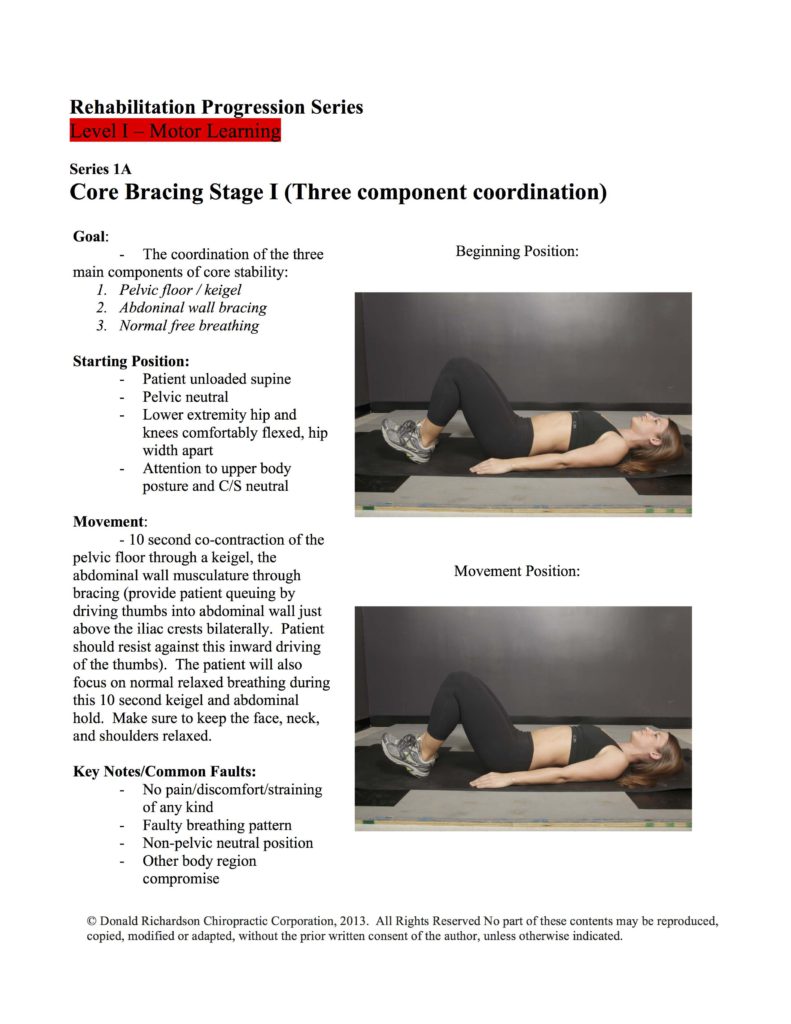
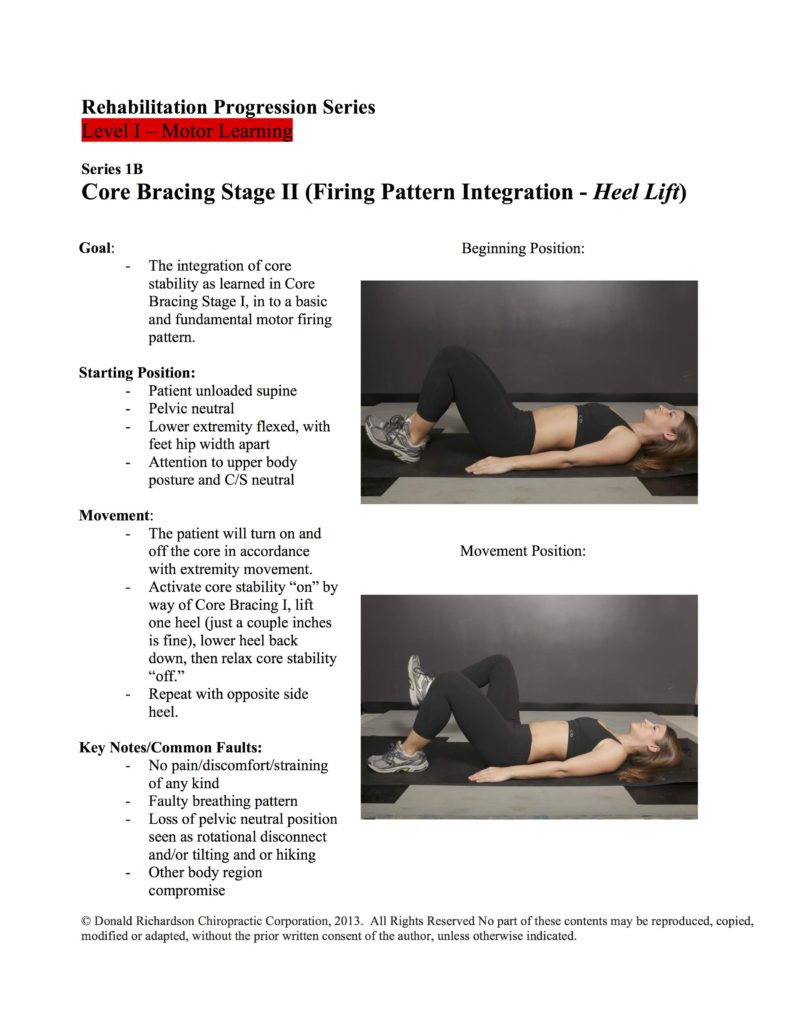
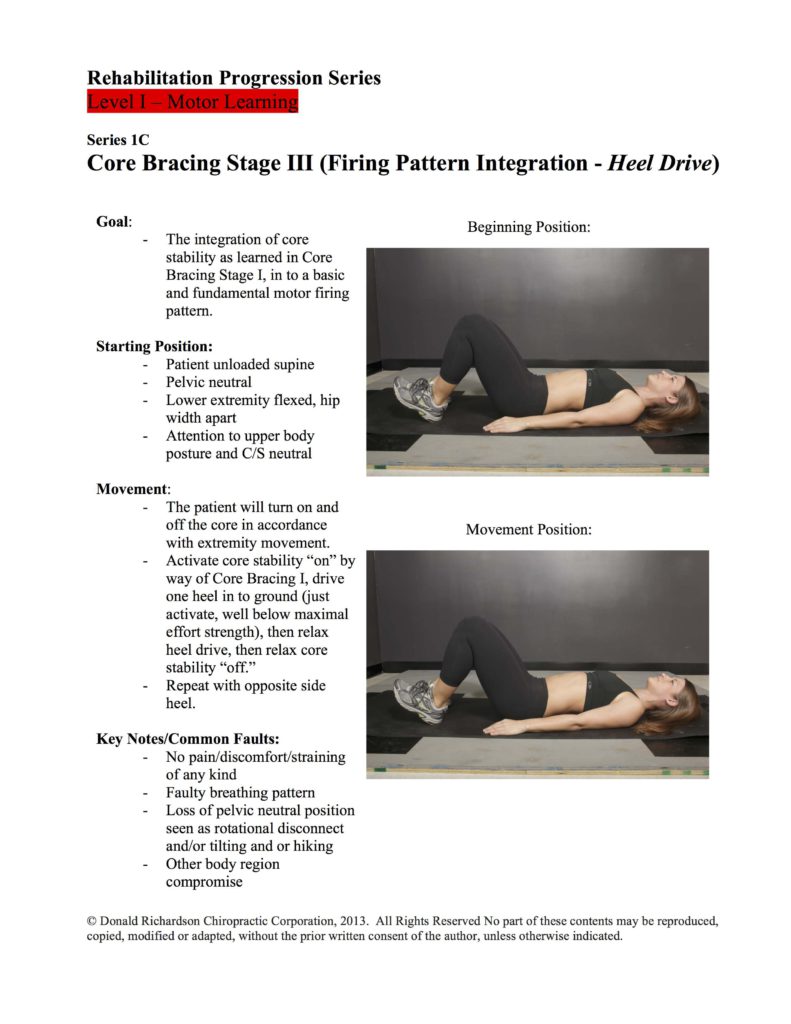
There is not a whole lot of movement that occurs between the sacroiliac joints and the 1st lumbar vertebrae, (your core) or if there is a lot of movement then you’re probably suffering from an injury or setting yourself up for one. One of the first things to address in lumbar spine or sacroiliac dysfunction is that although motion is good, I agree, it is not the desired attribute for this particular area of the body, as a matter of fact the sacroiliac joints have been shown in studies to have only 2-5 degrees of motion, max! The approach here is to teach pelvic control through a rudimentary stepwise process. Here is the first 3 steps to the motor learning of pelvic control:
LUMBOPELVIC ACTIVATION:
The activation of the lumbopelvic region is a transitional and progressive portion to the control portion we just highlighted above in the first 3 stages of lumbopelvic motor control. If you cannot control the core then you should not be attempting to activate it through peripheral movements. I may be remiss to assume that when I mention core activation the image in your head is not someone hammering away at sit-ups, leg lifts, and other lumbar spine insensitive movements that cause compression and shearing that is detrimental to low back health. Here are a two of Chads staple activation exercise progressions, Bird Dog and Dead Bug variations. These sample activation exercises must be utilized in the early acute phase of injuries and can be incorporated into any movement preparation warm-up.
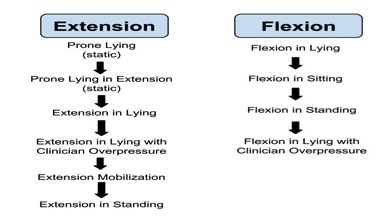
MCKENZIE’S PROTOCOL:
The Mckenzie protocol we used with Chad was the extension protocol. All disc injuries have position intolerances and the non-technical way to address it using these protocol systems is to utilize which of the positions is more favorable. In a clinical setting I do not use all of the philosophy that the McKenzie method teaches but I do use it as a piece in my holistic approach. The simple way I incorporate at home therapy using this school of thought is to put the patient into the 2 positions in the McKenzie protocol; static prone position (lumbar passive, patient resting on elbows), or child’s pose (hands in front with legs tucked under and glutes sitting on heels). Whatever position the patient would prefer to stay in all day is what I will have them perform at home. This picture depicts the progression through the extension protocol Chad performed, minus the clinician-assisted steps.
HIP/ANKLE MOBILIZATION:
Creating a mobile lower extremity hip and ankle complex is a necessary task when dealing with any lumbopelvic condition, the hip more directly and for the activity specific requirements for Chad and his mechanism of injury the ankle is an important area. As I mentioned previously there are certain areas of the body that need to be mobile and areas that need to be stable. Almost every lumbar spine injury that is not related to some acute traumatic accident, you will find a discrepancy in the stable vs. mobile relationships. Typically what will present is the hip and ankle complex is not mobile enough and the lumbopelvic region is too mobile. The hip complex is made up of a number of different soft tissue structures and a full divulgence into a comprehensive approach to hip mobility will be for another time. For this instance a sample of Chad’s mobility exercises are mostly band-assisted movements and self-administered manual therapy (i.e. foam rolling). The Mulligan Concept is the foundation for the banded mobilizations that I teach my patients. Here is a video with a few of the mobilizations that we utilized for hip and ankle mobility and a video for ankle mobility. Keep in mind that much of the tissue quality change is being made with the manual therapy procedures that I wrote about in my part 2 passive care article.
This is a snippet into a longer 6-9 month time frame for rehabilitating the lumbar spine. At just 4 weeks however Chad was able to do some scaled down training progressions as we progressed forward with the rehabilitation plan above. The key to a successful speedily recovery is a multifaceted approach or a holistic approach if you will. The aspects of mental readiness and nutritional fortitude are part of this holistic approach but commentary on that is for another time. From Diagnosis, to Treatment plan and rounding it all off with rehabilitation that is movement preparation and GPP based will get you, your patients or clients back to your sport or lifestyle activity quick.
Dr. Jason Reynolds is 1 of 200 Board certified Chiropractic Sports Physicians, a small portion of the chiropractic field that is dedicated to the conservative management of sports injuries and enhancement of sports performance. Dr. Jason is Partner of Body Dynamix Chiropractic and Performance and operator/practitioner of Body Dynamix OC. He also works as a medical provider for USA Men’s Field Hockey and USA Beach Volleyball. Contact Jason at [email protected]Website, Facebook, Twitter